Bipolar I vs. Bipolar II: What’s the Difference?
Living with bipolar disorder or watching someone you love struggle with it can feel confusing, overwhelming, and sometimes even frightening. While both Bipolar I and Bipolar II share the hallmark mood swings of mania or hypomania paired with depression, they are not the same condition. Understanding the differences is essential for getting the right diagnosis, treatment, and support.
In this article, we’ll break down what sets Bipolar I apart from Bipolar II, explore symptoms, causes, and treatment options, and answer the most common questions people have, so you can feel informed, empowered, and ready to take the next step toward better mental health.
What is Bipolar Disorder?
Bipolar disorder is a mental health condition marked by extreme mood shifts, ranging from episodes of high energy and euphoria to deep depression. These fluctuations are more than just the ups and downs everyone experiences; they can significantly affect work, relationships, and daily functioning.
At its core, bipolar disorder is defined by:
Manic or hypomanic episodes: Periods of elevated mood, energy, or irritability.
Depressive episodes: Periods of sadness, hopelessness, or lack of motivation.
Bipolar disorder isn’t a one-size-fits-all condition. That’s why experts classify it into different types, the most common being Bipolar I and Bipolar II.
What is Bipolar I Disorder?
Bipolar I disorder is the more widely recognized form, often associated with full manic episodes.
Key Features of Bipolar I
Mania: Lasts at least 7 days, or is severe enough to require hospitalization. During mania, people may feel euphoric, need little sleep, talk excessively, make risky decisions, or experience racing thoughts.
Depressive Episodes: These typically last at least 2 weeks and include feelings of deep sadness, fatigue, guilt, or loss of interest in activities.
Severity: Episodes can disrupt daily life, work, and relationships significantly.
👉 Example: Someone with Bipolar I might spend days without sleep, impulsively spend large sums of money, or feel invincible during a manic phase, only to crash into a major depressive episode later.
What is Bipolar II Disorder?
Bipolar II disorder is often misunderstood as a “less severe” form, but that’s not accurate. Instead of full mania, people with Bipolar II experience hypomania, a milder form of elevated mood. However, the depressive episodes tend to be more frequent and longer-lasting than in Bipolar I.
Key Features of Bipolar II
Hypomania: Similar to mania but less severe and shorter (lasting at least 4 consecutive days). Hypomania doesn’t cause hospitalization or extreme impairment, but can still lead to poor decisions.
Depressive Episodes: Usually more intense and persistent than in Bipolar I, often leading to functional impairment.
Misdiagnosis Risk: Because hypomania is less disruptive, many people with Bipolar II are misdiagnosed with major depression, delaying proper treatment.
👉 Example: A person with Bipolar II may have bursts of high energy and creativity (hypomania), but the depressive episodes dominate their life, making it difficult to function normally.
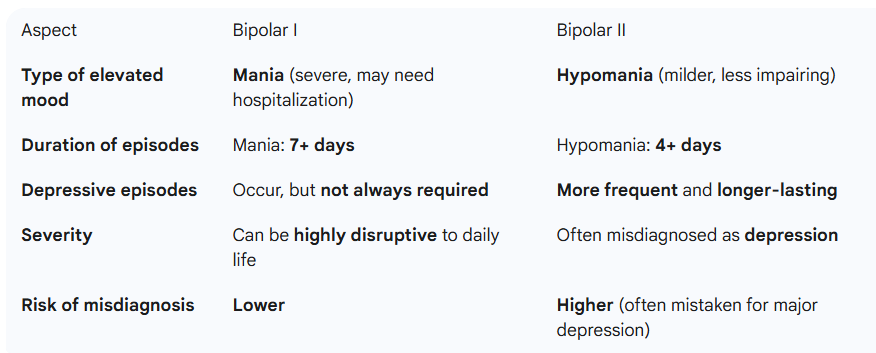
Bipolar I vs. Bipolar II: Key Differences
The biggest difference between the two is mania in Bipolar I vs. hypomania in Bipolar II, with Bipolar II having more recurring depression.
Signs & Symptoms: How to Recognize Each Type
Bipolar I Symptoms
Extreme energy and activity levels.
Decreased need for sleep.
Inflated self-esteem or grandiosity.
Risky behavior (spending, sex, substance use).
Severe depressive episodes (not always present).
Bipolar II Symptoms
Hypomanic phases (increased productivity, talkativeness, confidence).
Intense, recurring depression.
Fatigue, hopelessness, and loss of interest in daily life.
Irritability during hypomania or depression.
Higher risk of being mistaken for “just depression.”
While both types involve mood swings, the severity and duration of elevated episodes differ significantly.
Causes & Risk Factors of Bipolar Disorders
Like most mental health conditions, bipolar disorders don’t have a single cause. Instead, they stem from a combination of factors:
Genetics: If a close family member has bipolar disorder, your risk is higher.
Brain Chemistry & Structure: Imbalances in neurotransmitters like dopamine and serotonin play a role.
Environmental Triggers: Stress, trauma, substance abuse, or major life events can trigger episodes.
Age of Onset: Most cases develop in late adolescence or early adulthood.
Understanding these risk factors helps reduce stigma and emphasizes that bipolar disorder is a medical condition, not a personal weakness.
Diagnosis: How Doctors Differentiate Between Bipolar I & II
Diagnosing bipolar disorder isn’t as simple as checking off a list of symptoms; it requires a thorough clinical evaluation. Doctors and mental health professionals rely on:
Medical History: Reviewing symptoms, episode patterns, and family history.
Psychological Assessments: Structured interviews and questionnaires to identify manic, hypomanic, or depressive episodes.
Differentiation Between Mania & Hypomania: This is the key factor in distinguishing Bipolar I from Bipolar II.
Exclusion of Other Conditions: Thyroid problems, substance abuse, or medication side effects can mimic bipolar symptoms.
Self-diagnosis is unreliable. If you suspect you or someone you love may have bipolar disorder, seeking professional help is crucial.
Treatment Options for Bipolar I & Bipolar II
While there’s no cure for bipolar disorder, effective treatment can stabilize moods and allow individuals to live fulfilling lives.
Medications
Mood stabilizers (e.g., lithium): Cornerstone of treatment.
Antipsychotics: Often used for manic episodes.
Antidepressants: Sometimes prescribed but with caution, as they can trigger mania in Bipolar I.
Therapy
Cognitive Behavioral Therapy (CBT): Helps identify negative thought patterns.
Interpersonal and Social Rhythm Therapy (IPSRT): Focuses on stabilizing daily routines and sleep.
Psychoeducation: Empowers patients and families with knowledge.
Lifestyle & Self-Care
Regular sleep schedule.
Healthy diet and exercise.
Stress management techniques (mindfulness, meditation).
Avoiding alcohol and recreational drugs.
👉 While treatments for Bipolar I and II overlap, the management of mania vs. hypomania often shapes the treatment plan.
Living With Bipolar Disorder: Coping & Support
Living with bipolar disorder can be challenging, but with the right strategies and support, people can thrive.
Daily Management: Tracking moods, maintaining routines, and setting realistic goals.
Support Systems: Family, friends, and support groups are invaluable.
Education: Understanding the condition reduces stigma and helps with adherence to treatment.
Early Intervention: Recognizing early warning signs of an episode can prevent escalation.
Remember, bipolar disorder does not define who you are; it’s just one part of your life.
Conclusion
Both Bipolar I and Bipolar II involve significant mood changes, but the key difference lies in the type of elevated mood episode: mania in Bipolar I versus hypomania in Bipolar II. While Bipolar I can cause more acute disruptions due to mania, Bipolar II often comes with longer-lasting and more frequent depression.
Understanding these differences is the first step toward better management, effective treatment, and compassionate support. If you suspect you or someone you care about might have bipolar disorder, don’t wait; seek professional bipolar disorder treatment now. With the right care, people with bipolar disorder can live healthy, balanced, and meaningful lives.
FAQs
Q: Can Bipolar II turn into Bipolar I?
Ans: No. Bipolar II doesn’t “become” Bipolar I. However, if someone with Bipolar II experiences a full manic episode, the diagnosis may be updated to Bipolar I.
Q: Which is more severe: Bipolar I or II?
Ans: Bipolar I is often considered more severe due to mania, which can lead to hospitalization. However, Bipolar II can be equally debilitating because of frequent, intense depression.
Q: Can you have both Bipolar I and II?
Ans: No, a person can only be diagnosed with one type based on their episodes.
Q: How long do episodes last in Bipolar I vs II?
Bipolar I: Mania lasts at least 7 days, depression lasts at least 2 weeks.
Bipolar II: Hypomania lasts 4+ days, depression lasts 2+ weeks, and tends to be more chronic.
Q: Is Bipolar II easier to live with than Bipolar I?
Ans: Not necessarily. While Bipolar II doesn’t include full mania, the depressive burden is heavier, making it equally challenging.