Borderline Personality Disorder vs Bipolar Disorder: How to Tell the Difference
If you’ve ever wondered why Borderline Personality Disorder (BPD) and Bipolar Disorder are so often confused, you’re not alone. Both conditions involve intense mood changes, emotional distress, and disruptions to daily life, yet they are fundamentally different mental health disorders. Misunderstanding these differences can lead to delayed diagnosis, ineffective treatment, and unnecessary frustration.
In this article, we will explore Borderline Personality Disorder vs Bipolar Disorder in a clear, human, and practical way. You’ll learn how BPD differs from Bipolar 1 and Bipolar 2, why their symptoms overlap, and how professionals accurately diagnose each condition.
What Is Borderline Personality Disorder (BPD)?
Borderline Personality Disorder (BPD) is a personality disorder that affects emotional regulation, self-image, and interpersonal relationships. People with BPD experience emotions more intensely and more rapidly than others, which can make even small situations feel overwhelming or painful.
BPD is not about “moodiness” or weakness; it reflects long-standing emotional and behavioral patterns that usually begin in early adulthood and affect daily functioning.
Common Symptoms of BPD
Common symptoms of Borderline Personality Disorder include:
Intense and rapidly changing emotions
Extreme fear of abandonment, whether real or perceived
Unstable and intense personal relationships
Impulsive behaviors such as overspending, substance use, or risky actions
Self-harm or suicidal thoughts in some individuals
Chronic feelings of emptiness
Difficulty controlling anger
These emotional shifts often occur within hours or days and are frequently triggered by relationship conflicts or feelings of rejection.
Causes and Risk Factors of BPD
There is no single cause of BPD. Instead, it develops from a combination of factors, including:
Childhood trauma, abuse, or emotional neglect
Genetic vulnerability to emotional sensitivity
Differences in brain areas responsible for emotion regulation
Invalidating or unstable early environments
What Is Bipolar Disorder?
Bipolar Disorder is a mood disorder characterized by extreme mood episodes that range from emotional highs (mania or hypomania) to deep lows (depression). Unlike BPD, these mood episodes are not usually triggered by daily events and tend to last much longer.
People with Bipolar Disorder may function relatively well between episodes, especially when properly treated.
Types of Bipolar Disorder
Bipolar 1 Disorder
Bipolar 1 Disorder is defined by the presence of at least one manic episode. Mania is a severe mood state that may include:
Extremely elevated or irritable mood
Excessive energy and activity
Decreased need for sleep
Grandiose thinking
Risky or impulsive behaviors
Manic episodes typically last at least seven days and often require hospitalization due to their intensity.
Bipolar 2 Disorder
Bipolar 2 Disorder involves:
Hypomanic episodes, which are milder than full mania
Major depressive episodes, which can be severe and long-lasting
Many people with Bipolar 2 struggle more with depression than hypomania, making the condition harder to identify and sometimes mistaken for unipolar depression or BPD.
Common Symptoms of Bipolar Disorder
Mood episodes lasting days, weeks, or even months
Periods of high energy followed by deep depression
Significant changes in sleep, focus, and activity levels
Impaired judgment during mood episodes
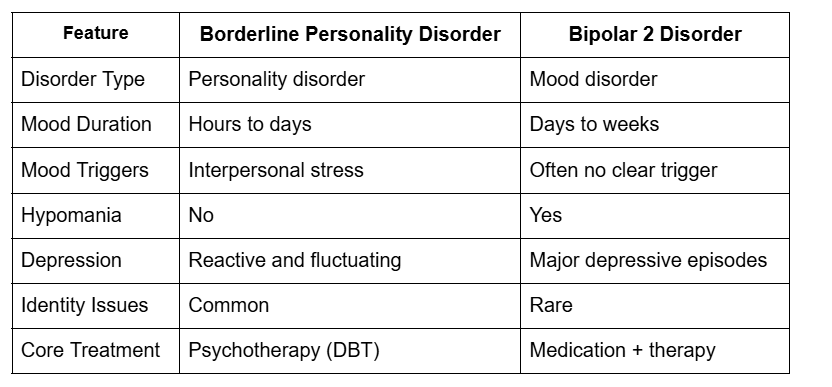
Bipolar vs Borderline Personality Disorder: Key Differences
Although Bipolar Disorder and Borderline Personality Disorder share overlapping symptoms, they are fundamentally different mental health conditions.
Mood Duration and Triggers
Borderline Personality Disorder: Mood swings are rapid and often triggered by interpersonal stress, rejection, or fear of abandonment.
Bipolar Disorder: Mood episodes last much longer and may occur without any external trigger.
Emotional Patterns
BPD involves chronic emotional sensitivity and instability.
Bipolar Disorder involves episodic mood changes with periods of emotional stability in between.
Identity and Relationships
People with BPD often struggle with unstable self-image and intense, unstable relationships.
Bipolar Disorder does not typically cause identity disturbance or chronic relationship instability.
Borderline Personality Disorder vs Bipolar 2
Borderline Personality Disorder (BPD) and Bipolar 2 Disorder are often confused because both involve mood instability and depressive symptoms. However, the nature, duration, and triggers of mood changes are very different. In BPD, emotional shifts are rapid and reactive, while Bipolar 2 is defined by distinct mood episodes, especially major depression and hypomania.
People with Bipolar 2 typically experience longer periods of low mood, whereas individuals with BPD struggle more with relationship-driven emotional reactions and identity instability.
Borderline Personality Disorder vs Bipolar 1
Borderline Personality Disorder and Bipolar 1 Disorder differ significantly in severity and clinical presentation, despite some overlapping behaviors such as impulsivity and emotional intensity. The defining feature of Bipolar 1 is the presence of full manic episodes, which do not occur in BPD.
While emotional reactions in BPD are usually triggered by fear of abandonment or relationship conflict, manic episodes in Bipolar 1 often develop independently of external circumstances and can lead to hospitalization.
Which Is Worse: Bipolar Disorder or Borderline Personality Disorder?
One of the most searched questions online is: which is worse, bipolar disorder or BPD? The honest answer is that neither condition is inherently worse, but each presents its own challenges.
The severity of either disorder depends on:
Symptom intensity
Access to proper treatment
Individual coping skills
Support systems
How Bipolar Disorder Can Impact Life?
Bipolar Disorder can be severely disruptive during manic or depressive episodes. Manic episodes, especially in Bipolar 1, can lead to financial problems, damaged relationships, legal trouble, or hospitalization. Depressive episodes can be long-lasting and debilitating.
How Borderline Personality Disorder Can Impact Life
BPD often affects daily life through emotional pain, unstable relationships, fear of abandonment, and identity confusion. While mood shifts may be shorter, the chronic emotional distress can feel constant and exhausting without treatment.
Rather than asking which condition is worse, a better question is: which condition is being accurately diagnosed and effectively treated? With proper care, both conditions can become manageable.
Can You Have Borderline Personality Disorder and Bipolar Disorder?
Yes, it is possible to have both Borderline Personality Disorder and Bipolar Disorder at the same time. This is known as comorbidity and can make diagnosis more complex.
When both conditions occur together:
Mood symptoms may be more intense
Emotional regulation becomes more challenging
Treatment plans must be carefully tailored
This is why professional assessment by a qualified mental health provider is critical.
Treatment Options for BPD and Bipolar Disorder
Both conditions benefit from professional intervention, but approaches differ.
Borderline Personality Disorder Treatment
Dialectical Behavior Therapy (DBT): Focuses on emotional regulation and coping strategies.
Cognitive Behavioral Therapy (CBT): Helps change harmful thought patterns.
Group Therapy: Builds interpersonal skills and support networks.
Medication: May be used to manage co-occurring anxiety, depression, or impulsivity, but is not a primary treatment.
Bipolar Disorder Treatment
Mood Stabilizers: Lithium, valproate, or lamotrigine to prevent mood swings.
Antipsychotic Medications: Used in manic or severe depressive episodes.
Psychotherapy: Cognitive Behavioral Therapy, family therapy, or psychoeducation supports adherence and coping.
Lifestyle Management: Regular sleep, exercise, and stress management are crucial.
Living With BPD or Bipolar Disorder
Managing life with either disorder requires a combination of therapy, medication (if prescribed), and support systems.
Coping Strategies
Maintain consistent therapy sessions.
Follow prescribed medications.
Keep a mood diary to track triggers and patterns.
Build a support network of understanding friends or family.
Practice self-care, mindfulness, and stress reduction techniques.
Tips for Families and Caregivers
Educate yourself about the disorder.
Encourage treatment adherence.
Set boundaries and practice patience.
Avoid personalizing mood-driven behaviors.
Summary
Exploring the difference between Borderline Personality Disorder and Bipolar Disorder is essential for accurate diagnosis, effective treatment, and improved quality of life. While symptoms may overlap, key distinctions in mood duration, triggers, identity issues, and treatment approaches set the conditions apart.
With the right support therapy, medication, lifestyle management, and a strong support system, individuals with either condition can manage symptoms and thrive.
If you or a loved one struggles with emotional instability or mood episodes, seek professional help today from our psychiatric nurse practitioner at Serenity Telehealth. Early diagnosis and treatment make a significant difference in recovery and overall well-being.
FAQs
Q1. Is BPD the same as bipolar disorder?
Ans: No. BPD is a personality disorder characterized by emotional instability and relationship issues, while bipolar disorder is a mood disorder with distinct episodes of mania or hypomania and depression.
Q2. Can BPD mood swings look like bipolar disorder?
Ans: Yes, rapid emotional shifts in BPD may seem like bipolar episodes, but BPD swings are usually short and triggered by relationships, whereas bipolar episodes are longer and more episodic.
Q3. Is Bipolar 2 less severe than BPD?
Ans: Severity depends on individual symptoms and life impact. Bipolar 2 can involve major depressive episodes, while BPD involves chronic emotional distress and identity instability.
Q4. Can someone have both BPD and bipolar disorder?
Ans: Yes. Comorbidity is possible and requires careful evaluation and personalized treatment.
Q5. Can BPD be cured?
Ans: There is no cure, but symptoms can be effectively managed with therapy and coping strategies, allowing for a fulfilling life.