Is Dermatillomania a Form of OCD? What You Need to Know
If you’ve ever found yourself repeatedly picking your skin and wondering why you can’t stop, you’re not alone, and you’re not weak. Dermatillomania, also known as skin picking or excoriation disorder, is a real mental health condition that affects millions of people worldwide.
One of the most common and confusing questions people ask is: Is dermatillomania a form of OCD, or is it something else entirely? The answer isn’t as simple as yes or no.
In this guide, we’ll break down the connection between dermatillomania and OCD, explore whether it can be linked to anxiety or ADHD, uncover possible genetic factors, and explain the most effective treatment options available today.
Is Dermatillomania a Form of OCD?
The short answer is: dermatillomania is not exactly the same as OCD, but it is closely related.
Dermatillomania, clinically known as excoriation disorder, is classified under the Obsessive-Compulsive and Related Disorders category in the DSM-5. This means it sits on the OCD spectrum, alongside conditions like trichotillomania (hair-pulling disorder).
However, dermatillomania does not always involve the classic intrusive thoughts that define traditional OCD. While OCD compulsions are usually driven by fear-based obsessions (such as contamination or harm), skin picking is often driven by urges, sensory discomfort, stress, or emotional regulation needs.
✔️ Dermatillomania is OCD-related, but not the same as having OCD
✔️ Some people have both conditions, others have dermatillomania alone
This distinction is important because it affects diagnosis, treatment, and self-understanding.
Is Dermatillomania OCD? Understanding the Overlap
Many people search for “Is dermatillomania OCD?” because the behaviors feel uncontrollable, just like compulsions in OCD.
Here’s how they overlap
Repetitive, compulsive behaviors
Difficulty stopping despite negative consequences
Temporary relief after performing the behavior
Feelings of shame, guilt, or distress
How they differ?
OCD behaviors are usually performed to neutralize intrusive thoughts
Dermatillomania behaviors are often automatic or sensory-driven
Skin picking may occur without conscious anxiety or fear
This overlap explains why dermatillomania is frequently misdiagnosed, or dismissed entirely.
Can Dermatillomania Exist Without OCD?
Yes. Absolutely.
Dermatillomania can occur independently, without a formal OCD diagnosis. Many people with excoriation disorder do not experience obsessive thoughts or ritualistic mental patterns associated with OCD.
Instead, skin picking may be linked to:
Emotional regulation
Stress relief
Boredom or restlessness
Sensory sensitivity
Habitual behavior patterns
That’s why effective treatment often focuses on behavioral awareness and habit reversal, not just anxiety reduction.
Could Dermatillomania Be Anxiety or ADHD Instead?
This is another extremely common and valid question.
Dermatillomania and Anxiety
While dermatillomania is not classified as an anxiety disorder, anxiety is one of its most common triggers.
People often pick their skin when:
Feeling overwhelmed
Experiencing chronic stress
Trying to self-soothe
Managing emotional discomfort
In these cases, skin picking acts as a coping mechanism, even though it ultimately causes harm.
Dermatillomania and ADHD
Dermatillomania is not ADHD, but the two frequently co-occur.
People with ADHD may be more prone to skin picking due to:
Impulsivity
Difficulty regulating attention
Sensory-seeking behaviors
Restlessness or under-stimulation
This explains why some individuals notice increased picking during periods of boredom or mental fatigue.
✔️ Dermatillomania can exist with OCD, anxiety, or ADHD
✔️ It is not automatically caused by any one condition
A proper evaluation looks at patterns, triggers, and motivation, not just labels.
Is There a Genetic Component to Dermatillomania?
Research suggests that genetics may play a role in dermatillomania, though it is not caused by genes alone.
Studies show that skin picking disorder tends to:
Run in families
Appear alongside other OCD-spectrum conditions
Share genetic traits related to impulse control and compulsive behaviors
This does not mean dermatillomania is inevitable if it runs in your family—but it may increase susceptibility when combined with environmental factors like stress or trauma.
What This Means for You?
Dermatillomania is not a personal failure
Biology, psychology, and environment all contribute
Effective treatment does not depend on genetics alone
What Is Excoriation Disorder?
Excoriation disorder is the clinical name for dermatillomania.
Diagnostic Features Include
Recurrent skin picking resulting in skin lesions
Repeated attempts to stop or reduce the behavior
Significant emotional distress or impairment
The behavior is not due to a medical condition or substance use
The disorder can affect any area of the body, including the face, arms, scalp, legs, and hands. Over time, it may lead to scarring, infections, and emotional withdrawal.
Dermatillomania Symptoms: How to Recognize Excoriation Disorder
Dermatillomania often goes unnoticed or is minimized as a “bad habit,” but it has clear and recognizable symptoms that go far beyond occasional skin picking.
Recurrent skin picking that causes sores, wounds, or scarring
Strong urges to pick that feel difficult or impossible to resist
Picking during stress, boredom, anxiety, or emotional distress
Picking becoming automatic or unconscious over time
Repeated attempts to stop, followed by relapse
Feelings of shame, guilt, or embarrassment afterward
In many cases, people go to great lengths to hide visible marks, avoid social situations, or wear clothing and makeup to cover the damage, further impacting mental health and self-esteem.
When Should You Seek Help for Dermatillomania?
Occasional skin picking is common. Dermatillomania becomes a disorder when it interferes with your life.
You should consider seeking professional help if:
Skin picking causes pain, infections, or permanent scarring
You feel unable to stop despite repeated efforts
The behavior affects work, relationships, or daily functioning
You experience emotional distress, anxiety, or depression related to picking
Early intervention can prevent long-term physical and emotional consequences.
Dermatillomania Treatment: What Actually Works?
The good news is that dermatillomania is treatable. Effective treatment focuses on understanding triggers and changing behavioral patterns, not on willpower alone.
1. Cognitive Behavioral Therapy (CBT)
CBT is the most evidence-based treatment for excoriation disorder. It helps individuals:
Identify triggers and patterns
Challenge unhelpful thought processes
Develop healthier coping mechanisms
2. Habit Reversal Training (HRT)
HRT is a specialized CBT technique and a cornerstone of dermatillomania treatment. It includes:
Increasing awareness of picking behaviors
Learning competing responses (alternative actions)
Reducing environmental triggers
3. Acceptance and Commitment Therapy (ACT)
ACT helps individuals:
Accept urges without acting on them
Reduce shame and self-criticism
Focus on values-driven behavior rather than control
4. Medication (When Appropriate)
Some individuals benefit from medications such as SSRIs, especially when dermatillomania co-occurs with OCD, anxiety, or depression. Medication is most effective when combined with therapy.
5. Supportive Strategies
Stress management techniques
Mindfulness and grounding exercises
Covering triggers (bandages, gloves) during early recovery
Tracking patterns and urges
Important: Treating only the skin (creams, dermatology visits) without addressing the psychological component is rarely effective long-term.
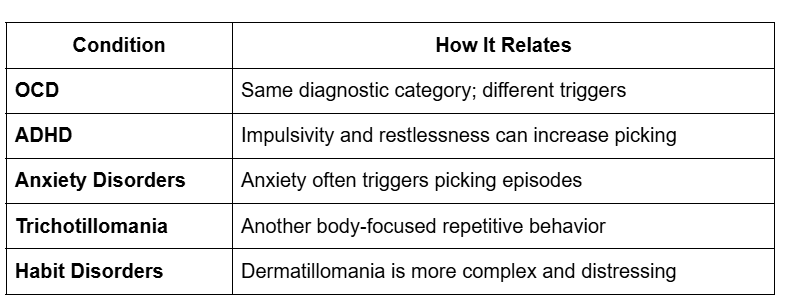
Dermatillomania vs OCD, ADHD, and Similar Conditions
Understanding how dermatillomania differs from related conditions can help reduce confusion and self-blame.
Many individuals have more than one condition, which is why treatment must be personalized.
Is Dermatillomania Genetic or Learned?
Dermatillomania is best understood through a biopsychosocial model:
Biological factors: genetics, brain chemistry
Psychological factors: emotional regulation, impulse control
Social factors: stress, trauma, environment
This means dermatillomania is not a choice, not a flaw, and not a failure of self-control.
Final Thoughts
✔️ Dermatillomania is not classic OCD, but it is closely related
✔️ It can exist with OCD, ADHD, anxiety, or on its own
✔️ Genetics may increase vulnerability, but they do not determine outcome
✔️ Effective, evidence-based treatments are available
If you struggle with skin picking, help is possible, and recovery does not require perfection, only progress.
If dermatillomania is affecting your physical health, emotional well-being, or quality of life, consider reaching out to our licensed psychiatric nurse practitioner for skin picking disorder. The sooner you seek support, the sooner healing can begin.